Factors That Affect Endometrial Thickness and What They Mean
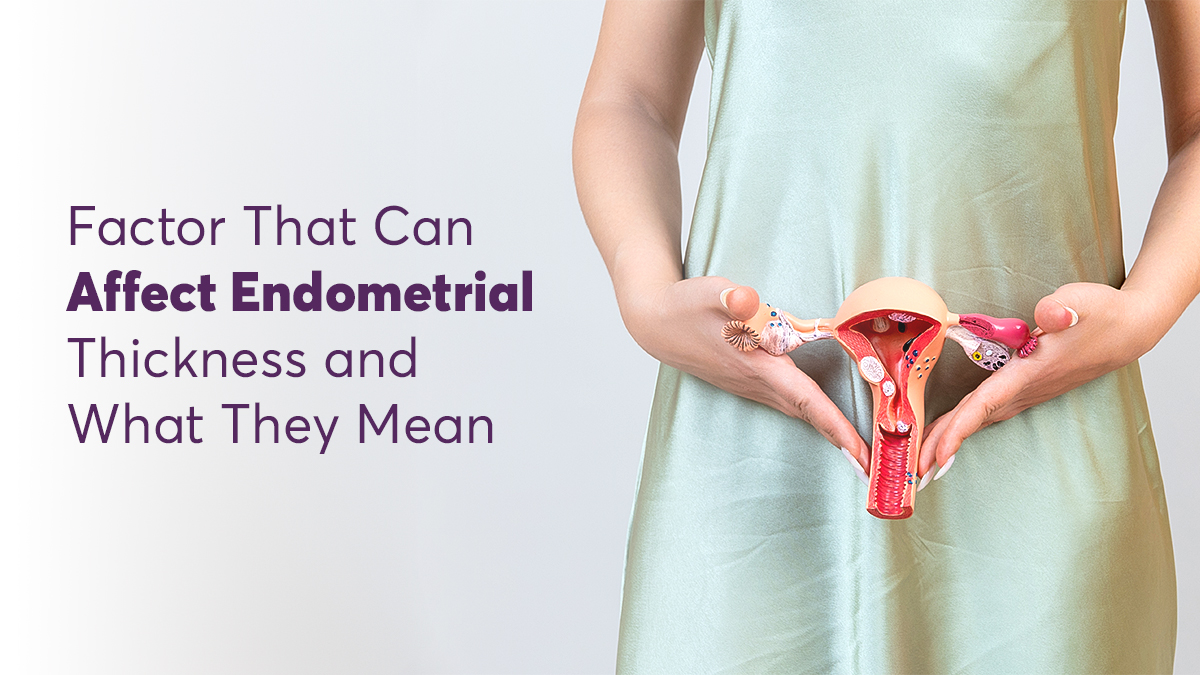
Not knowing the real reason behind your inability to conceive can be heartbreaking. A medical checkup can help identify whether your endometrial thickness is coming in the way of your getting pregnant. Affecting over 190 million women of reproductive age as per WHO’s data, increased thickness or thinning of the endometrium is a manageable condition. However, early diagnosis and management are important to prevent pregnancy issues. Do not worry even if you are diagnosed after failing to conceive. The condition can be handled with some lifestyle changes and medication. You may be able to carry your baby to term with medical assistance. Learn how to identify the symptoms and proceed with its treatment.
Understanding Endometrial Thickness
The endometrium is the inner lining of the uterus. A balance of the female hormones, estrogen and progesterone, helps maintain the correct thickness of the endometrium. Its thickness varies throughout the menstrual cycle. The normal size of the endometrium lining in mm is:
- During menstruation: 1 to 4 mm
- Follicular phase till ovulation: 10 to 16 mm
- Luteal phase: 16 to 18 mm
The most appropriate endometrial thickness for pregnancy is 8-15 mm. It grows to provide a healthy environment for the embryo to attach itself, and for the fetus to grow.
Measuring Endometrial Thickness
The thickness of the endometrial lining is assessed via:
Transvaginal Ultrasound
This is a popular method in which the doctor inserts a small device through the vagina, using a flexible tube, and then uses sound waves to assess the lining. This procedure is painless and quick.
Hysteroscopy
Here, the doctor uses a camera to see if the thickness of your endometrial lining is abnormal. This is also a painless and quick procedure. However, some discomfort during insertion and extraction of the tube is normal.
Sonohysterography
Under certain medical conditions, inserting a tube to observe the uterine lining may be difficult. In such cases, your doctor may suggest sonohysterography. The doctor injects a saline solution to evaluate the uterine cavity during the sonogram. The procedure may cause occasional cramping, which subsides after a few days and can be managed with painkillers.
Factors Affecting Endometrial Thickness
Many factors cause abnormal endometrial thickness:
Hormonal Influences
Excessive estrogen and low progesterone cause endometrial thickening (endometrial hyperplasia), while low estrogen or excessive progestin causes thinning.
Medical Conditions That Impact Endometrial Thickness
Endometrial thinning may be a result of:
- Age: As women get closer to menopause (35-40), the endometrial lining thins.
- Prolonged treatment: Especially for endometrial hyperplasia, or any prolonged medications
- Chronic Endometritis
- Endometrial TB
- Ashermann Syndrome
- PCOD: If the eggs do not mature, the estrogen levels remain below normal, causing thinning of the uterine lining.
- Iatrogenic – Repeated DnCs
- Idiopathic
- Endometriosis: Lining growth outside the uterus
Reasons for Endometrial Thickness:
- PCOS: May reduce progestin exposure, preventing the shedding of the lining.
- Perimenopause: Before menopause, women may not ovulate regularly, which causes progesterone levels in the body to decline.
- Breast or ovarian cancer medications: Tamoxifen, a drug used to treat breast cancer, mimics estrogen. If you have undergone a treatment without progestin support, the uterine lining may be unusually thick.
You might also be at a high risk of developing endometrial issues if there is a family history of reproductive cancers or PCOS/PCOD, even if you don’t have it. Additionally, smoking, drinking, obesity, and anorexia may cause endometrial problems.
Uterine fibroids and scarring of the uterine tissue (Asherman’s Syndrome) due to a previous miscarriage(s) or surgery may also cause abnormal endometrial thickness.
Medication and Treatments for Endometrial Thickness
Lifestyle changes, such as ensuring a balanced diet, exercise and stress reduction, can positively impact endometrial health. In fact, healthcare professionals recommend such lifestyle changes as part of fertility treatments. Thin endometriosis may lead to difficulties in conceiving or miscarriages. Optimal thickness helps support the baby’s nutrition in the womb.
The most popular treatments for improving fertility and endometrial health are:
Hormonal Therapy: Your doctor may suggest supplements oral or vaginal or intra uterine hormone treatment to restore the estrogen-progestin balance.
Treatment for Thickened Endometrium: Down-regulation of the estrogen and progesterone levels.
Endometrial Scratching : Scratching the endometrial lining lightly close to ovulation stimulates growth and facilitates thickening.
Assisted Reproductive Technologies (ART): ARTs, such as IVF, are successful only with a healthy endometrium. Often, such procedures may start with endometrial treatment to ensure that the embryo has ideal conditions to grow after fertilisation.
Monitoring and Managing Endometrial Health
Since you cannot measure endometrial thickness at home, check whether your menstrual cycle is normal without excessive pain. If you have been trying to get pregnant without success, facing menstrual issues, or see any symptoms of PCOS/PCOD, get a medical consultation. Your doctor will examine the endometrial lining and then guide you regarding the normal size of the endometrium in mm and the future course of treatment.
Conclusion
Healthy endometrium is critical to the success of IVF and other fertility treatments. The good news is that with technological advancements, endometrial conditions can be diagnosed and managed to improve your fertility and well-being.


fill up the form to get a
Free Consultation
Avail 0% interest on EMI
All Procedures | No Upper Limit
Frequently Asked Questions
When should I worry about endometrial thickness?
Is it OK to have thickened endometrium?
Is 4.5 mm endometrial thickness normal?
How we reviewed this article:
- Current Version
- August 1, 2024 by Oasis Fertility
- June 26, 2024 by Oasis Fertility