Everything you need to know about Fallopian Tube Blockage and Infertility
Infertility affects a staggering number of people. All genders experience infertility due to causes known and unknown. Blockage in the fallopian tubes is one of the prevalent causes of female infertility.
Blockage in the fallopian tubes accounts for a cause of infertility in approximately 30% of women worldwide.
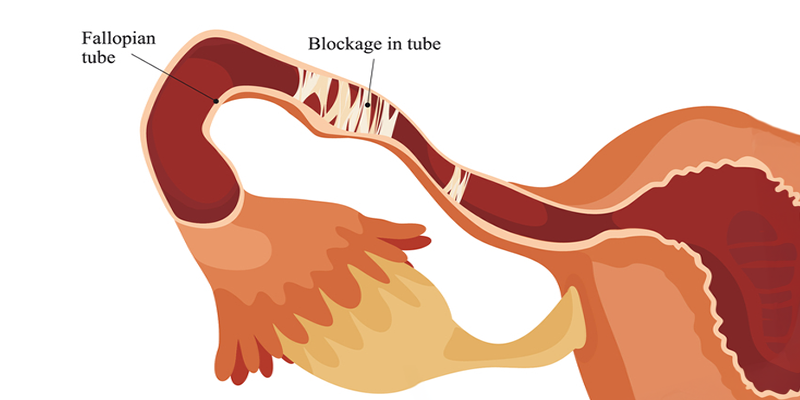
What are fallopian tubes?
The fallopian tubes are the bridges that connect the ovaries and the uterus.
It plays a major role in the process of conception.
It allows the egg to travel from the ovaries to the uterus. The sperm travel upwards from the uterus through the fallopian tubes to meet with the egg which may result in the potential fertilization of the egg.
The fertilized egg travels through this bridge and gets implanted in the uterus resulting in a pregnancy.
Reasons behind blockage in fallopian tubes
Of all the range of reasons, below are a few factors that result in a tubal blockage:
- Presence of scar tissue due to infections (such as pelvic inflammatory disease and STIs)
- History of abdominal surgery – appendix removal surgery, Ectopic pregnancy
- Endometriosis
- Inflammation in the uterus and fallopian tubes
- Birth defects and abnormalities of the uterus and the fallopian tubes
- Fibroids or polyps in the uterus
Signs that you might have blocked fallopian tubes
Symptoms of a fallopian tube blockage depend on the root cause of the blockage.
For example, in the case of Endometriosis, the individual may experience heavy and painful periods.
There is mild to regular pain on one side of the abdomen in the case of Hydrosalpinx.
Some women may experience pain in the pelvic region randomly or during their period.
However, upon diagnosis, this condition can be managed and treated.
Diagnosis of blocked fallopian tubes
Blocked fallopian tubes are difficult to identify due to their root cause-specific symptoms. Usually, the condition is undiagnosed until an individual faces difficulty getting pregnant.
Tests to diagnose blocked fallopian tubes
The most commonly used tests to diagnose blocked fallopian tubes:
- Hysterosalpingogram or HSG is an X-ray test, in which a safe nontoxic dye is injected into the uterus to detect the blockages in the fallopian tubes.
- Sonohysterogram, commonly called a sonogram, is an ultrasound test used to view the inside of the uterus. It creates a computer image using sound waves.
- Laparoscopy famously known as Keyhole surgery in which a small cut is made in the body to insert a tiny camera that helps to view the inside of the abdomen.
Effect of blocked fallopian tubes on fertility
As a consequence of tubal blockage, fertilization of the egg does not occur. This condition is characterized a tubal factor infertility.
In a few cases even if fertilization occurs (due to partially blocked tubes), the blockage in the fallopian tube restricts the movement of the fertilized egg to the uterus, leading to an Ectopic pregnancy.
Although, it is still possible for an egg to get fertilized and result in pregnancy if there is a blockage in only one of the fallopian tubes.
Related Read – What Do You Need to Know About Tubal Factor Infertility?
Treatment options for Blocked fallopian tubes:
As mentioned, one can get pregnant if the fallopian tubes are partially blocked, or if one tube is open. However, the risk of an ectopic pregnancy is high in the case of a partially blocked tube.
In case of a complete blockage in both the fallopian tubes, the chances of conceiving without treatment are far lower.
Fallopian tube blockage treatment options are based upon
- The age of the individual
- Type/cause of the malformation
- Location of the blockage
In case of a pelvic infection diagnosis, antibiotics are prescribed.
In conditions where surgery is required, there are some alternatives:
- Laparoscopic surgery to repair fallopian tubes: This is a minimally invasive procedure that opens blocked fallopian tubes. A small incision is made in the belly, to insert a tiny telescope that sends images for the doctor to operate. The recovery time is usually 2-3 days.
- Hysteroscopic surgery to repair fallopian tubes: This sends the telescope through the cervix. Since there is no incision, the recovery time is shortened to 24 hours.
- Laparoscopic surgery to remove fallopian tubes. In case of severe damage, the fallopian tubes may need to be removed. Following this surgery, IVF treatment can help to conceive.
The chances of conceiving after surgery depend upon:
- Age
- Partner’s sperm health
- The level of fallopian tube damage
Conception With IVF Intervention
In cases where surgery is not recommended or in the event of an unsuccessful surgical outcome, the IVF or In – Vitro Fertilization (IVF) treatment may be recommended.
During the IVF process, mature eggs from the ovaries are collected and fertilised by sperms in a lab. One or more of the fertilised eggs (embryos) are placed in the uterus for the baby to grow. A full cycle of IVF treatment takes 2-3 weeks.
IVF can be done with a couple’s own eggs and sperm or taking embryos from a donor. Your age and overall health are important factors determining the success of the IVF treatment.
The doctor may recommend intrauterine insemination (IUI) instead of IVF. In the IUI treatment, sperms are put into the uterus to fertilise the eggs. This increases the number of healthy sperms that reach the fallopian tubes.
Conclusion
It’s possible to have your dream of having a baby, even in case of a fallopian tube blockage with the right intervention at the right time.
Always consult your doctor about the treatment options available and suitable to you, to understand your chances at having a healthy and safe pregnancy.


fill up the form to get a
Free Consultation
Avail 0% interest on EMI
All Procedures | No Upper Limit
Frequently Asked Questions
Can you get pregnant with one blocked fallopian tube?
Can a blocked fallopian tube cause infertility?
Can you get pregnant after fallopian tube removal?
How we reviewed this article:
- Current Version
- August 28, 2024 by Oasis Fertility
- June 4, 2024 by Oasis Fertility
- May 30, 2024 by Oasis Fertility
- January 4, 2024 by Oasis Fertility
- August 28, 2023 by Oasis Fertility
- August 25, 2023 by Oasis Fertility
- August 16, 2023 by Oasis Fertility
- August 8, 2023 by Oasis Fertility